Approach to Upper Gastrointestinal Subepithelial Lesions – Explained Simply
When people undergo an endoscopy for stomach issues, sometimes doctors discover something unexpected — small bumps or growths under the inner lining of the stomach, esophagus, or intestines. These are called subepithelial lesions (SELs).
Most of the time, SELs are harmless and don’t cause symptoms. But in certain cases, they can be cancerous or turn into something more serious if left unchecked. This is why understanding, diagnosing, and managing SELs properly is so important.
What Are Subepithelial Lesions (SELs)?
SELs are growths that occur beneath the surface lining of the stomach, esophagus, or intestines.
They are usually discovered accidentally during an endoscopy.
Around 1 in every 100 endoscopies may show an SEL.
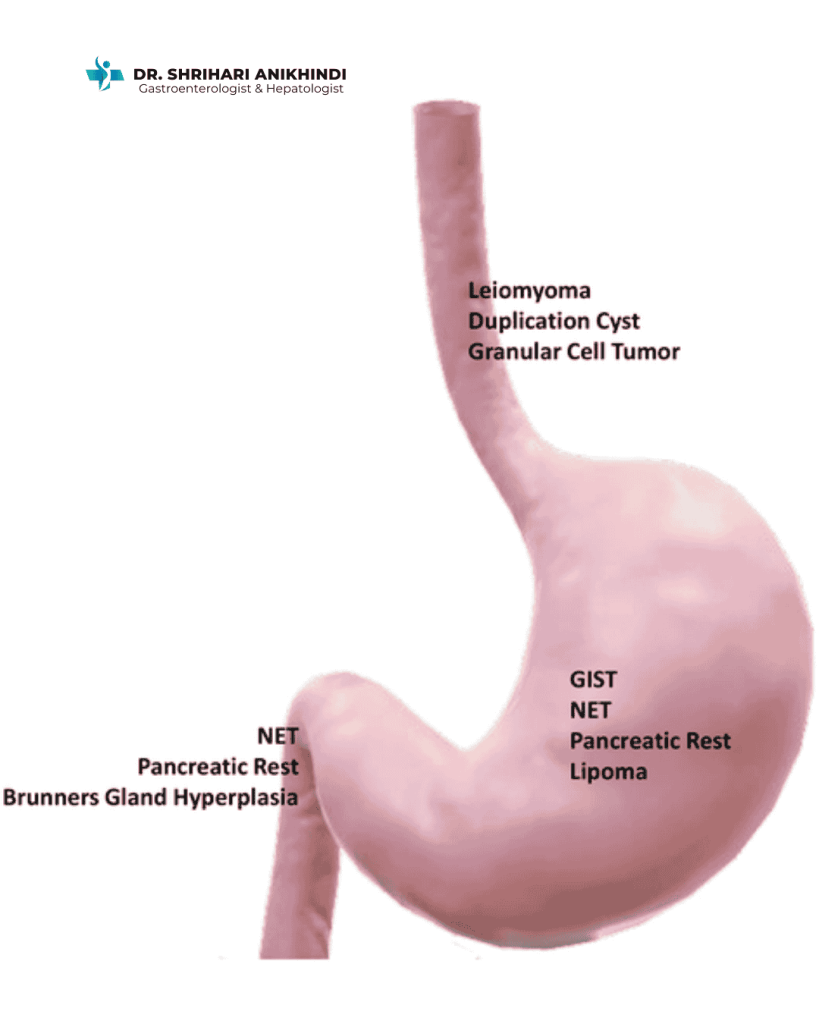
Types of Subepithelial Lesions
Not all SELs are the same. Common types include:
GISTs (Gastrointestinal Stromal Tumors) – may be cancerous.
NETs (Neuroendocrine Tumors) – sometimes malignant.
Leiomyomas – usually harmless muscle tumors.
Lipomas – fatty tissue growths, mostly benign.
Pancreatic rests – small areas of pancreatic tissue.
Duplication cysts – fluid-filled sacs.
👉 The important thing to know: most SELs are harmless, but about 15% can be malignant. That’s why proper evaluation is critical.
How Are SELs Diagnosed?
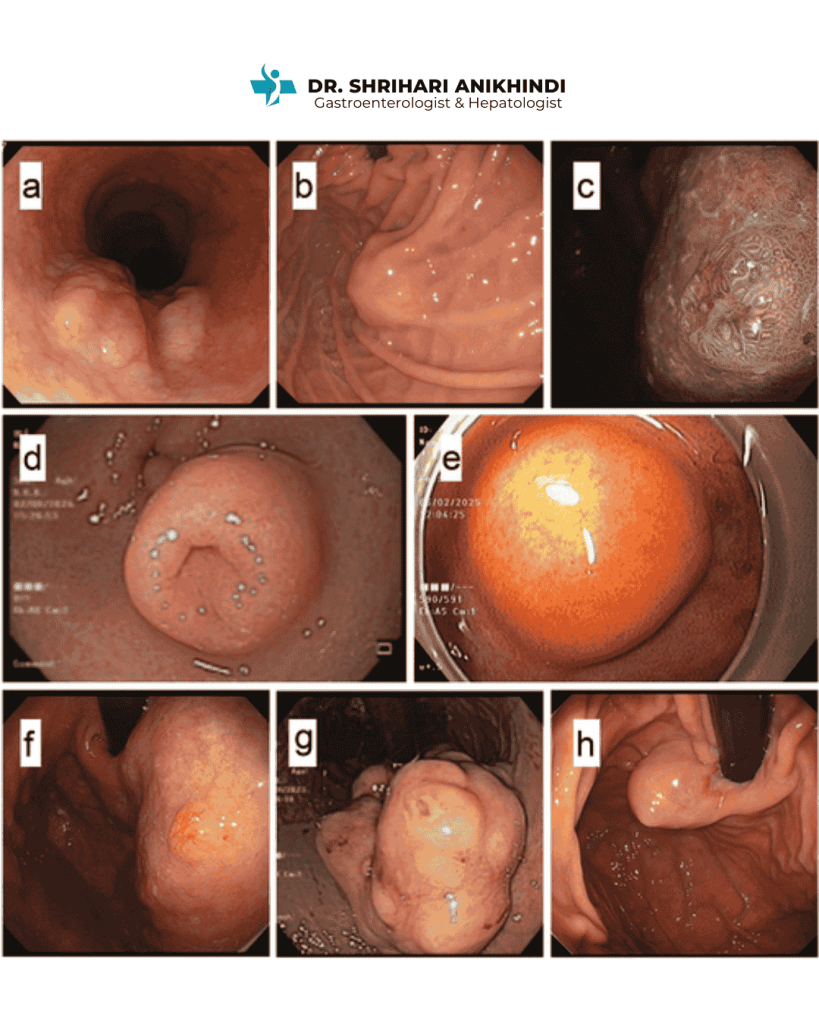
Traditionally, a simple endoscopy only shows a “bump” but cannot confirm what type of lesion it is.
The gold standard today is Endoscopic Ultrasound (EUS):
Works like an ultrasound probe attached to the endoscope.
Shows where exactly the lesion is located (which layer of the stomach wall).
Helps guide a biopsy (tissue sample) for accurate diagnosis.
Modern Biopsy Methods:
EUS-guided Fine Needle Aspiration (FNA) – older method.
EUS-guided Fine Needle Biopsy (FNB) – newer and more accurate for diagnosis.
Treatment and Management
Treatment depends on the type, size, and risk level of the lesion:
Benign SELs (like lipomas, small cysts): Often don’t need treatment, just observation.
High-risk SELs (like GISTs, large NETs): Need to be removed either by advanced endoscopic methods or surgery.
Small, uncertain SELs: Monitored over time with follow-up endoscopies or scans.
👉 The goal is to avoid unnecessary surgery while making sure dangerous lesions are caught early.
Future of SEL Diagnosis and Treatment
Dr. Shrihari’s article also highlights exciting future directions:
AI and machine learning – can help doctors interpret endoscopic images more accurately.
New biopsy tools – improving precision of tissue diagnosis.
Molecular diagnostics – deeper understanding of tumor behavior.
These advancements mean patients will get quicker, safer, and more reliable results in the coming years.
Why This Matters for Patients
Most SELs don’t cause obvious symptoms, but they can sometimes lead to bleeding, abdominal pain, or anemia.
Ignoring them could delay treatment of early cancers.
Modern endoscopy and EUS make diagnosis safe, accurate, and minimally invasive.
Expert Insights from Dr. Shrihari Anikhindi
Dr. Anikhindi’s expertise in endoscopy and liver care has helped thousands of patients in Delhi. By contributing to international journals, he shares valuable insights that improve medical knowledge and patient care globally.
👉 You can read his full research article here: [https://www.tandfonline.com/eprint/XGZBBE5KKA5CG4J4UGNA/full?target=10.1080/17474124.2025.2519161#d1e257]